
又是一年清明時節,梅雨淒淒。但又正值暖春,萬物復蘇,生機盎然。每逢四月,想起已經不在的他們,便會更加珍惜身邊健在的我們。生老病死乃人之常情,如何舒適度過生命的最後一刻,是香港中文大學醫學院那打素護理學院陳裕麗教授(Professor Helen Chan)斟酌了接近20年的課題。
香港以長壽為傲,曾七年蟬聯全球最長壽地區。在追求人均壽命長度的同時,晚期照顧的資源及配套也應同時備受關注,保障生命晚期的質素。本期Cubic Zine聚焦Helen及其團隊在華人地區首創的預設照顧計劃及其成效與國際影響力。
臨終兩難決定:拔喉棄急救?躺著為活死人?
預設醫療指示(Advance Directives)的概念早於1967年由一為捍衛人權的律師 Luis Kutner於美國安樂死協會(Euthanasia Society of America)的會議上提出。之後由於在審議能否從植物人身上撤除呼吸機的法庭案件的判決(詳見 Karen Quinlan事件),加州於1976年率先通過《自然死法案》(Natural Death Act),保障個人設立「生前預囑」(Living Will)的權利,允許個人決定自己臨終或意識不清時是否繼續維生治療(如心肺復甦術、人工輔助呼吸)。假如他日不幸陷入病重昏迷,醫護人員將停止施行意願人早已拒絕的維生治療,但這不等同於施行安樂死。雖然兩者的原意都是為減少病人所受的痛苦,但是實施安樂死實質上是以醫療手段直接結束病人的生命,有違醫德,在大部份國家都被界定為不合法,而停止對病人施行無效維生治療,是順其自然地讓病人逝去。
但是美國的經驗反映單純推動簽署法律文件,未能促進意願人事先與家人或醫護人員討論有關晚期照顧的想法,同類的法庭案件在接下來的二十年仍然不斷重演。因此,預設照顧計劃(Advance Care Planning, 簡稱ACP)的概念開始引起關注,希望意願人可先與家人溝通自己對未來醫療或個人照顧的意願,才再簽署預設醫療指示。

於2000年初期,西方國家推動預設照顧計劃也處於起步階段。閱讀極其有限的文獻時,Helen發覺:「西方國家的做法很單刀直入。一開始就會問:你想不想接受心肺復甦法,你覺得臨終的時候要接受一些怎樣的治療?我感覺在我們華人文化下沒辦法這樣問。」
在華人地區開展預設照顧計劃絕非易事。現今華人對中國文化「孝」概念的詮釋側重於延長壽命,當病患者病入膏肓,大多數人仍然會堅持用盡所有治療方式搶救,深怕放棄治療便無法讓病患者堅持到最後一刻,留下遺憾——人們常常陷入這兩難處境。同時華人對「死亡」這一話題較為忌諱,且溝通模式也偏委婉含蓄,直接照搬西方的做法肯定不行。
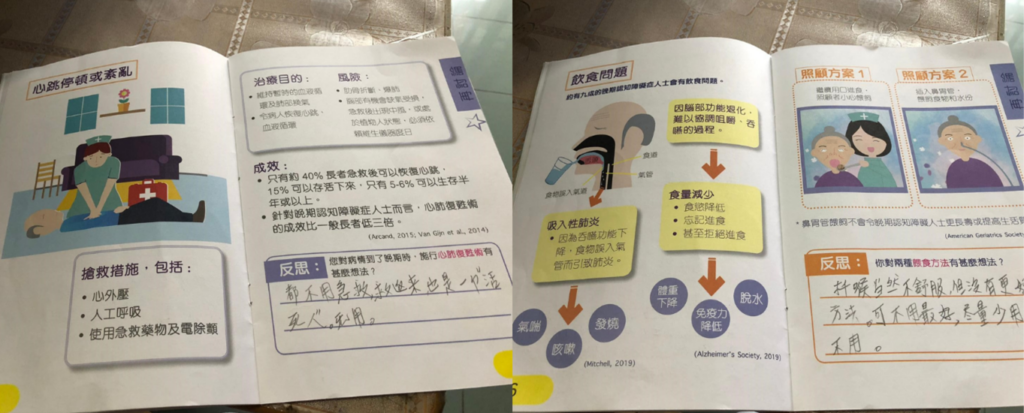
Helen研發在地化版本十分注重以人為本,因地制宜,充分考慮華人的文化和溝通模式:護士或社工作為第三方先與意願人透過傾談建立互信,循序漸進切入正題;再邀請意願人的親人介入,協助意願人將自己的想法告訴親人。
團隊中老年學出身再進修成為社工的Shirley形容預設照顧計劃「不只是醫療方面的決定,也是對整個人生的反思。」在與意願人的訪談中,護士或社工先帶著意願人回顧過往的人生經歷,例如自己的健康情況、親友離世時的情況,從而促進個人反思自己對晚期照顧的價值觀,然後展望未來,自己對日後照顧的意願。
Helen鼓勵同事不要擔心講多錯多,「我們現在提出有關晚期照顧方面,有些病人或家人可能會覺得比較難接受,甚至生氣到投訴我們。但是現在鼓起勇氣講一句,就可以幫到家庭先做好心理準備,如果要將代作決定的責任交給家屬,他可能會內疚一世。 」
化低谷成人生轉捩點
曾在院舍與老人科病房工作,Helen見到太多長者臨終前仍接受無效的維生治療,也親身參與無數次搶救之中。「我是護士背景,當年畢業就等於失業,慶幸獲得在家附近一家院舍聘成護士。院舍內很多長者都是瞓床,像是植物人的狀態,靠一些治療維生,例如鼻胃管餵奶。後來有機會進醫院工作,又看到另一番境象:自己親身經歷為很多病重的長者做搶救,令我反思急救的意義在哪裡?自己與家人老了,是不是也要接受這樣的生活?晚期照顧怎樣可以做好一些?」。
Helen於2009年加入中大。她的研究計劃名為「吾」可預計,靈感來源於與長者交談時,他們感慨「以後嘅嘢就唔可以預計嘅」。「唔可預計」表示不可預計。把「唔」變作意為「我」的「吾」,則把否定變為肯定,強調了個人對生命的掌握,賦權予每個人決定如何為自己的生命畫上句號。

知識轉移項目基金(Knowledge Transfer Project Fund, KPF)為Helen照亮了黑暗,帶來黎明的曙光。「我一路都很appreciate知識轉移辦公室。它很敢於試不同的東西。當我通過其他途徑拿不到funding,我就鼓起勇氣嘗試申請KPF,好感恩它給了我很多機會。」通過兩期KPF資金,「吾」可預計有了自己的網頁,也拍攝微電影引發大眾對此話題的關注,並且發展了實證為本的ACP培訓課程。
從家福會到立法會
在Helen的全力推進下,2017年起,香港家庭福利會(家福會)的預設照顧計劃應運而生。Helen為提供服務的護士、社工等同事進行培訓;也在每次訪談前後請參與者填寫問卷,分析結果,從而改進服務。2021年獲維拉律敦治.荻茜慈善基金額外撥款資助,計劃進一步擴展服務,參與者可於預設照顧計劃後簽署包括預設醫療指示、持久授權書、平安紙/遺囑的「平安三寶」。其中「持久授權書」授權受權人在授權人神智不清時照顧其財務事項。
由於預設醫療指示只在疾病末期、持續植物人或昏迷狀態及晚期不可逆轉生存受限的三類情況生效,家福會的項目之服務對象只針對60歲以上患致命疾病、80歲以上高齡、領取綜援或低收入三類人士。而本港有望今年完成立法的《維持生命治療的預作決定條例草案》將賦予所有18歲以上的人士有自主權,可提早為如何跨過人生的終點線敲定方案。《條例草案》主要包括預設醫療指示和不作心肺復甦術命令兩個部分,以「慎入易出」作為原則。「慎入」確保訂立者簽訂的過程中需有兩名見證人在場,「易出」則允許訂立者有精神行為能力時可隨時撤銷之前簽訂的指示。
根據今年一月初的立法工作計劃,《條例草案》預計於今年第二季恢復二讀辯論及三讀。醫務衞生局指法例通過後,將進行一年半的過渡期,並同時向醫護界、社福界和市民宣傳教育。 4月26日,Helen也將在社區講座中為大眾普及預設醫療指示,分享經驗。
有溫度地簽文件
在立法會法案委員會上,有議員提出「病人在簽署前可能與家屬無溝通」的擔憂,因為簽署過程只需一名醫生和一名無利益關係的人見證。若家屬不理解病人的意願,可能會質疑病人於文件上所作的決定,將這個燙手山芋反而拋給了醫護人員。醫院管理局臨床倫理委員會主席謝文華的回應強調簽署過程「會請病人的家人一起參與」,讓家屬親耳聽到病人的意願。
推廣預設照顧計劃的同時,Helen其實更想促進家庭成員間的溝通:「我不是一開始就推廣簽這份文件。如果我們只是推簽文件,一定會有很多紛爭,就像為了遺囑打官司。所以我自己更加盡力推廣的是家庭的分享、溝通。」


在家福會推行預設照顧計劃的陳君悅女士也坦言自己每天收到很多關於簽署文件的諮詢。「我們做project最想做的其實不是要簽多少文件,而是簽的過程希望意願人與家人有溝通。家人知道其意願才可以代作最符合當事人的決定。」團隊成員、曾經在急診室工作的劉智傑先生也從臨床角度吐露心聲:「即使沒有法律文件,家人肯開口在醫院與醫生講「我的爸爸媽媽是不想這樣的」,其實都可以讓長者得到好的晚期照顧。」
團隊成員楊智恩博士也分享了在服務時聽到的故事:有位獨居、患有早期認知障礙症的婆婆有10個子女,每一晚都有子女與她一起吃飯,就因為他們都擔心婆婆很孤獨,所以子女輪流陪婆婆吃飯:星期一阿哥,星期二阿妹……這樣的溫情事例令她感動不已:「在每個人生故事上,我自己的得著很多。見證著他們可以透過預設照顧計劃更加了解對方,更加知道未來這條路應該怎麼走,其實作為醫護人員都很開心很滿足。」
「自主善終」風氣漸盛
2008年,Helen的博士論文發表,分析了「讓我說說」計劃(「吾」可預計的前身)的成效與啟示。計劃為本地 121位居住於安老院舍的長者進行預設照顧計劃,以storytelling的方式帶領他們回顧人生經歷 (我的故事),從而幫助他們釐清自己對生命的看法 (我的看法),及為生命最後一程進行規劃 (我的意願),成首套為華人社會量身定制的ACP方案,此後這方式也陸續受到其他亞洲地區應用。
新加坡衛生部於2011年啟動名為「Living Matters」的預先護理計劃項目,由衛生部屬下的獨立機構護聯中心執行。預先護理計劃可於實體醫院或線上進行。他們制定的計劃手冊,主題也是分為我的反思、我的看法、我的護理目標及我的下一步,讓意願人預先了解自己的狀況及計劃內容,並將這些資料上傳至國家電子醫療紀錄。
推行初期的2011年至2015年期間,僅5,100新加坡人訂立預先護理計劃。隨著宣傳力度逐步加大,以及社會對於「死亡」的討論更加開放,截止2023年5月尾,已有超過36,600新加坡人訂立預先護理計劃。
台灣於2019年1月6日正式施行《病人自主權利法》(簡稱病主法),賦予病人「知情」和「做選擇」的自主機會。民眾可通過簽署預立醫療決定(Advance Decision),保障未來處於五種臨床條件時得以善終。病人需與二親等內之親屬,在醫院完成預立醫療照護諮商(Advance Care Planning, ACP)後,方可簽署決定。諮商團隊由1名醫師、1名護理師以及1名心理師或社工組成。每次諮商平均60至90分鐘。
今年1月6日,台灣病主法施行滿5週年,逾6萬人簽署預立醫療決定,但只佔成人人口不到1%。諮商團隊人力資源不足是運作上的一大難題。即使疫情後大量民眾湧入門診自願簽署,現有人力也難以應付。
北京生前預囑推廣協會亦於2013年成立,於中國各省市推廣計劃晚期照顧的概念。而於2022年深圳亦為生前預囑立法,尊重意願人事先簽署文件拒絕於晚期接受維生治療的決定。
積極推動亞洲地區ACP發展——以堅持聚人心
Helen將繼續投身於公眾教育,在更多人身上埋下種子;也希望醫社合作之餘,有更多政商界、法律界、媒體界的持份者參與其中,為種子提供合適的土壤與氣候,形成生態。春來秋去,靜候其生根發芽,碩果累累,接下來便是交給時間了。
相關資料:
「賽馬會安寧頌」安寧照顧講座《維持生命治療的預作決定條例草案》知多啲 – 社區講座系列
第七場 :
| 日期 : | 2024年4月26日 |
| 時間 : | 下午4時正至5時30分 |
| 地點 : | 香港灣仔軒尼詩道十五號溫莎公爵社會服務大廈2樓202室 |
| 講者: | 《維持生命治療的預作決定條例草案》的背景與主要條文 醫務衞生局副秘書長2 李力綱先生 |
| 講者: | 香港中文大學醫學院那打素護理學院教授 陳裕麗教授 |
| 主持人 : | 香港大學賽馬會安寧頌計劃講師 李淑霞姑娘 |
| 活動流程 : | 點撃這裡 |
| 對象 : | 港島區公眾人士 |
| 費用 : | 免費參加 |
| 語言 : | 廣東話 |
| 報名 : | 點撃這裡 |
編輯:中大研究及知識轉移服務處、黃翔堃(中大全球研究學生、知識轉移大使)



