When we are young and healthy, we have control over our lives. We can choose our jobs, partners, and where we live, creating an ideal life for ourselves. But when we reach old age and experience physical and mental decline, can we still make the best decisions for our own lives, especially at the end of life? Professor Jean Woo, the Director of The CUHK Jockey Club Institute of Ageing, shared the practical situation of discussions on end-of-life care among healthcare professionals and patients.
Professor Woo graduated from the University of Cambridge in the UK and is a pioneer in the field of geriatrics. She has been involved in the development of geriatric services at the New Territories East Cluster of Hospitals, establishing a day hospital for the elderly in 1985, and serving as the head of the Department of Medicine and Geriatrics at the Shatin Hospital from 1993 to 2012. Over the past forty years, she has gained extensive practical experience in healthcare and has seen the needs of many patients and their families.
Healthcare professionals’s avoidance becomes a barrier to discussing “Advance Care Planning”
Professor Woo pointed out that in reality, there are still healthcare professionals in hospitals who avoid discussing end-of-life care. Due to their heavy workload, they lack the time and space to have conversations with patients and their families, making it difficult to initiate discussions on Advance Care Planning (ACP). She shared an example of a patient’s complaint, saying, “I know that my condition is not curable, but why do doctors not even look at me during their rounds and just focus on my medical records?” Professor Woo emphasized that the public is very receptive to ACP discussions and has a good understanding of it. However, doctors are busy with urgent surgeries and daily consultations, rarely proactively discussing the expected prognosis and explaining end-stage treatment options to patients. Nurses also hesitate to initiate complex conversations with patients without crossing the line with doctors.
In addition to public hospitals, nursing homes also face similar challenges. According to a 2023 study by the Faculty of Medicine at the Chinese University of Hong Kong, about 70% of elderly residents in nursing homes have cognitive impairment. As residents gradually lose their ability to communicate, discussing ACP becomes a significant challenge, and staff in nursing homes often do not get involved in their medical decisions.
Effective communication is crucial, but how do we start?
Since 2016, Professor Woo has led the Jockey Club End-of-Life Care Training and Education Program in collaboration with the Hospital Authority. Over 20,000 healthcare professionals and social workers have been trained to deepen their understanding of palliative care and enhance their abilities in this area. The program focuses on role-playing and group discussions to help participants understand how to effectively communicate with patients and their families. The program team has also produced a series of instructional videos, such as “How to Deliver Bad News to Patients’ Families,” “How Healthcare Professionals Initiate Conversations about End-of-Life Care” (Speaker is Professor Helen Chan), and “Addressing Differences in Initiating Advance Care Planning.” These videos present the communication process of palliative care from different perspectives for healthcare professionals to reference. Additionally, the program educates patients, families, and the general public on how to face death, creating a more supportive environment for palliative care services in Hong Kong.
In 2021, the institute published a report titled “LIVE FREE DIE WELL: Building Capacity for End-of-Life Care in Hong Kong,” summarizing the achievements and outcomes of the program. Through regular public education activities conducted in hospitals, it was found that the general public is generally open to discussing palliative care, not only willing to deepen their understanding but also considering initiating ACP with their families at an earlier stage. However, they may not necessarily find suitable healthcare professionals to have these discussions, and sometimes they feel confused due to differing terminology and opinions among doctors from different departments. Healthcare professionals need to improve their communication skills, ensure that patients and their families receive adequate support, and initiate discussions with them early on instead of waiting until the last moment.
Professor Woo emphasizes, “You cannot set the instructions at the last moment of your life! You need to prepare as soon as possible.” Furthermore, healthcare professionals should have the understanding that initiating discussions on palliative care is not solely the responsibility of geriatric or palliative care specialists. On the contrary, members from different disciplines within the healthcare team should be able to discuss this topic.
“Advance Medical Directive” will be enacted, hoping for cooperation from various parties
Regarding the promotion of Advance Medical Directives (AMD), Professor Woo believes that capacity building for healthcare professionals is essential. “It’s not just a tick box exercise, where everyone fills out a form. It should be a patient-centered discussion,” she said.
The government recently published the “Advance Decision on Life-Sustaining Treatment Bill” in the Gazette, providing a legal framework for AMD and studying the use of electronic systems to sign and store directives. While legislative work is underway, there are still doubts and questions from patients and their families. Many are seeking information from relevant service units. Professor Woo reminds us that besides the mindset shiftof healthcare professionals, public education and awareness are equally important. The general public needs to understand the concept of AMD, its purpose, and the importance of having discussions with their families and healthcare providers. Open and honest communication is crucial to ensure that individuals’ wishes are respected and followed through in their end-of-life care.
In conclusion, Professor Jean Woo emphasizes the importance of effective communication in palliative care. Healthcare professionals need to initiate discussions on end-of-life care and Advance Care Planning with patients and their families early on, rather than waiting until the last moment. Training programs and educational initiatives can help enhance the communication skills of healthcare professionals and create a supportive environment for palliative care services. Public awareness and understanding of topics like AMD are also crucial for ensuring that individuals’ wishes are respected and fulfilled in their end-of-life care.
Edit by: ORKTS — Alice Fong (Communications Officer@InnoPort )
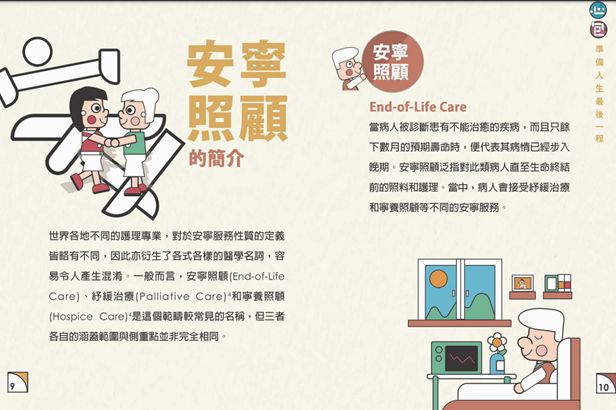
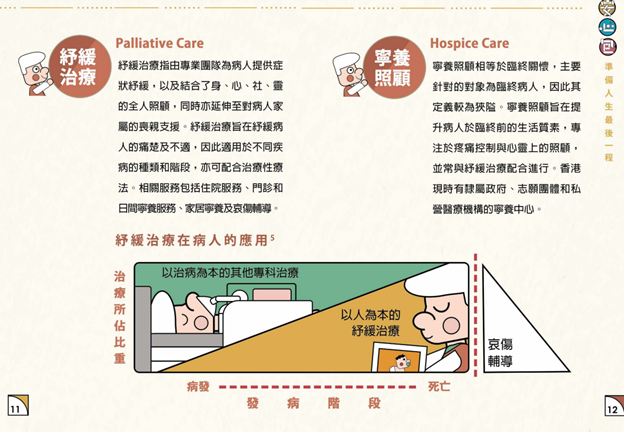
End of Life Care Resources Kit from Jockey Club End-of-Life Care Training and Education Program :